Navigating the Path to Wellness With Massage Therapy
from the AMTA:
It’s estimated that more than 51 million American adults discussed massage therapy with their doctors or health care providers in 2015.1

Stats like these tell us that more clients than ever view massage therapy as an integral part of their health care regime. In response, it’s essential that you understand when massage is indicated or contraindicated for specific pathologies.
How essential? Consider this: 20 years ago, massage for cancer patients was categorically judged unwise for fear that it accelerated the spread of the cancer.2 However, recent studies reverse this opinion, highlighting specific instances where massage is both indicated and highly beneficial for cancer patients. Similarly, researchers now feel that patients with any of the following five chronic medical conditions—or pathologies—can benefit from massage therapy.
ROCK YOUR RETAIL: KINESIOLOGY TAPE FOR CLIENT SELF-CARE
from Massage Magazine:
Kinesiology taping in massage practice is growing—and for very good reason.

Pain reduction, proprioception, movement mechanics and postural re-education; managing the fluid dynamics of swelling after an injury, surgical procedure, or related to lymphedema—these are some of the effects that kinesiology taping can provide.
As a practitioner, using this versatile tool in your office complements your soft tissue work in tangible ways and adds a very real perception of value and benefit for your client. This not only opens a gateway for client education, it empowers clients’ self-care.
Soma Massages at the Chicago Marathon
Every year it happens.
We take all of our students to volunteer in the Balboa Hospitality tent at the Chicago Marathon. In the weeks preceding the event various students will tell the teachers how nervous they are. These are actual people! What if they’re not up for the task? What if they start cramping and I can’t fix them? What if they need medical attention?
Every year we reassure them.
It’s going to be alright. We’ll review techniques before the race. We’ll be there to guide you. We won’t let you hurt anyone.
Every year they don’t believe us.

At 6am on race day most students are taking the train downtown to check in. Unlike most Sunday mornings, they notice that these trains are packed full of runners who are checking their phones one last time, checking their devices they’ll use for timing themselves, shoveling down a last minute peanut butter and jelly sandwich and telling family members what to do when they come running by. There are a handful of other commuters as well, bleary eyed, either going to work or coming home from a very late night out, some of whom are unimpressed by all the runners, some of whom attempt to make polite conversation with them. From the Blue Line we notice there are no runners training on the 606 this morning. The training is all done, and those runners who are not running the marathon choose to not go for their two mile jog this morning, either out of respect or embarrassment.
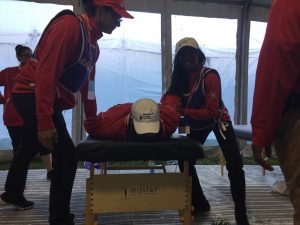
At 7am we all meet at the corner of Michigan Ave and 11th to check in and get our hats and jackets. They are red this year and have been for the past several years, since massage got lumped in with all medical practitioners. Everyone agrees the blue jackets looked cooler, and if we could get one of the gray ones we see some people have that would be even cooler still, but that the red ones are nice enough, and they’re free after all. Here at check in we get to see our current students as well as the alumni who have volunteered to work in the medical tent with Mike Hovi, our program director, and it’s always a nice reunion with familiar faces, getting to hear the successes they’ve had in their careers thus far.

Around 7:30am Hovi leads his therapists to the medical tent for orientation, and we take the current students to the Balboa Hospitality Tent where we’ll be working. Upon our arrival the students will pick the table they will use (at least at first) and who they will partner with. We have 45 tables this year for about 65 students, so at some point we’ll have to divide them up and have one person per table. We sip coffee and wait for Hovi to come back, and we watch the TV monitor in the main tent to see how the runners are doing.
At 8:30am Hovi comes back with the alumni and gathers everyone around two tables in the middle. He and Lambert demonstrate what to do if a runner catches a cramp in the hamstrings, in the calves, in the hip flexors or in the dorsiflexors. He talks everyone through basic techniques and stretches that they may or may not remember from their Sports Massage course. He reminds the students to talk to the runners, see if they’ve hydrated enough, make sure their feet aren’t bleeding and most importantly to make sure they know where they are. He encourages everyone to have a good time.

From 9am to 10am the students practice on each other, and we pace the tent correcting techniques, talking the students through stretches for particular muscles, cramp relief for various regions, and reminding them: feet on the table in supine, feet off the table in prone. Although most students seem cool enough, a few still have some nervousness to burn through. We will give those students the first runners, because it’s sink or swim time, and we know they almost always swim.
At 10:20 am the first athlete arrives. In fact we get three in quick succession. Two wheelchair athletes and one guy who said he was third place but none of us bothered to check if that was true.

Around 10:50 a woman comes in, her entire body looks like a cramp, and when she gets on the table she has multiple cramps and begins to suffer from hypothermia. Her body had been burning calories for 26.2 miles, and now that she’s stopped she’s lost that heat source, and she begins to shiver, almost violently. We move her table out into the sunlight, someone grabs a mylar blanket to cover her with, and with six or seven therapists (that’s twelve or fourteen hands) on her, everyone either actively engages in cramp relief or vigorous rubbing to generate heat. At some point her lips stop being as blue and an unnamed teacher jokes that she looks like a giant baked potato, but it’s a tough room. Eventually the med tent comes to claim her, and she gets some fluids and rest and is fine.
For the next hour a few of the faster runners come trickling in, and each is met by thunderous applause. We try to stagger the runners around the room, so even if the students aren’t working they have a good view of somebody who is, and perhaps this will put them into a good frame of mind. After the first twenty runners or so, when a good portion of the tables have people on them, the applause diminishes, and by 11:30, when nearly all the tables are full, the applause stops altogether.
For the next four and a half hours it’s nonstop massaging. It’s a hot day which makes the runners go slower, which means they trickle in at a slower rate this year. The faculty gets the runners to sign their consent form and then walks them over to the first free table they see. Communication eventually get whittled down to:
“How’re you feeling?”
“Sore.”
“Anything in particular?”
“My legs.”
“You don’t say. Well let me give you to so and so, she’ll take good care of you.”
And so on.
The faculty also monitors the room for any situations that get out of hand. We had only a few situations where the runners on the table wouldn’t stop cramping, and in all cases their problems were at least closer to being resolved when they left.
Every year it happens. These kids impress us. All the nerves fade away and they step up, they face their fears, and they work until their bodies ache.
Around 3:30, as a nice bookend to the day, we get another woman who won’t stop cramping and who begins to shiver violently. The students know what to do this time. We move her into the sun, we get her covered in mylar, the students start rubbing her vigorously, an unnamed teacher says it looks like we’re making Jiffy Pop, but it’s a tough room. She feels much better after a while, and even hugs her therapists, breaking down in tears for all the help. A satisfying moment is shared at that table.
At 3:45 we let our last runner into the tent, and as the last few runners are being worked on, we set the students to work breaking down the tables and carrying them out to the curbside for later pickup.
591 massages total.
Every year, the students come in afraid.
Every year they leave with a new found confidence in their work. They walk away wearing their red hats and red coats w ith pride. Some look sleepy, some still look wired from all the excitement, some pose for selfies, some text their rides to come get them, and some fall down in the grass, exhausted. They come into school the following week exchanging stories of this guy that cramped, or that woman who said she’d never felt better, or the how they went home after the marathon and slept for twelve hours straight, or how they had to go to work immediately following.
ith pride. Some look sleepy, some still look wired from all the excitement, some pose for selfies, some text their rides to come get them, and some fall down in the grass, exhausted. They come into school the following week exchanging stories of this guy that cramped, or that woman who said she’d never felt better, or the how they went home after the marathon and slept for twelve hours straight, or how they had to go to work immediately following.
Every year we are very proud of our students.
This year was no exception.
See more pics on our Facebook page.
What is Lady Gaga’s Chronic Pain? Fibromyalgia Explained
from Billboard
It's been an incredibly tough month for mother monster, Lady Gaga, who has very recently opened up about the battle she's facing with a chronic pain condition known as fibromyalgia. On Friday (Sep. 15) the singer began posting a series of photos from a hospital in Rio, Brazil explaining that she was unable to continue touring due to agonizing and severe physical pain. And while Gaga's Netflix documentary, Gaga: Five Foot Two, was supposed to look at her battle with pain, the actual reveal of her chronic illness came Monday (Sep. 18) on Instagram.

"I have always been honest about my physical and mental health struggles. Searching for years to get to the bottom of them. It is complicated and difficult to explain, and we are trying to figure it out. As I get stronger and when I feel ready, I will tell my story in more depth, and plan to take this on strongly so I can not only raise awareness, but expand research for others who suffer as I do, so I can help make a difference. I use the word "suffer" not for pity, or attention, and have been disappointed to see people online suggest that I'm being dramatic, making this up, or playing the victim to get out of touring. If you knew me, you would know this couldn't be further from the truth. I'm a fighter. I use the word suffer not only because trauma and chronic pain have changed my life, but because they are keeping me from living a normal life. They are also keeping me from what I love the most in the world: performing for my fans. I am looking forward to touring again soon, but I have to be with my doctors right now so I can be strong and perform for you all for the next 60 years or more. I love you so much," Lady Gaga said, announcing she needs to reschedule the European leg of her tour.
The news brings back into the spotlight a disease that has been often misunderstood by the public, one that is characterized by chronic pain and excessive fatigue with no known cause. Billboard spoke with the Mayo Clinic’s Dr. Arya Mohabbat and Connie A. Luedtke, R.N., nursing supervisor of the hospital’s Fibromyalgia Clinic, about what people should know.
Where pain lives
from AEON:
In the US, about 80,000 spine procedures fail each year , and one in five patients returns for another operation. Typically, second, third and fourth attempts have an even lower chance of success, and patients continue to require painkillers over the long term. Even the procedures that surgeons deem successful, because the bones fuse and look perfect on a scan, are often unhelpful to patients. In one study, two years after spinal fusion, patients’ pain had barely been reduced by half, and most patients continued to use painkillers. Given such unimpressive outcomes, the cost of treating back pain is unacceptably high. Spine surgery costs a fortune, but other approaches, including epidural steroid injections, physical therapy and chiropractic treatment, are also expensive.

Including direct medical expenses and indirect expenses such as lost earnings, spine care costs the US about $100 billion a year. In the UK, that tab is about £10.6 billion (c$13.6 billion). InAustralia, it’s A$1.2 billion (c$950 million). Many of these costs derive from the loss of productivity, as people take time off from work. Others result from the devastation wrought by addiction to prescription opioids. In Australia, between 1992 and 2012, prescription opioid dispensing increased 15-fold, and the cost to the Australian government increased more than 32-fold.
Pain falls into four basic categories. There’s nociceptive pain, the normally short-lived kind you feel when you accidentally slam your finger in the car door. There’s inflammatory pain, a response to damage or infection, resulting in a rush of small proteins called inflammatory cytokines to the site of the casualty. That pain has a habit of spreading, to affect everything in the vicinity. Beyond that, there’s neuropathic pain, known as ‘radiculopathy’. It results, usually, from an insult to a nerve, culminating in burning, tingling or shock-like sensations that travel the length of the affected nerve (sciatic pain is a good example).


 GET STARTED
GET STARTED



 Call Us
Call Us Get Information
Get Information Tour Soma
Tour Soma Apply Now
Apply Now